Small Intestinal Bacterial Overgrowth, commonly known as SIBO, is an increasingly recognized digestive disorder that affects the normal functioning of the gut. Although it has gained attention only in recent years, SIBO has likely been underdiagnosed for decades due to symptom overlap with other gastrointestinal conditions such as IBS, acid reflux, and food intolerances.
This comprehensive guide explains what SIBO is, why it occurs, how it is diagnosed, and the most effective treatment and management strategies, using evidence-based insights and practical explanations.
What Is SIBO?
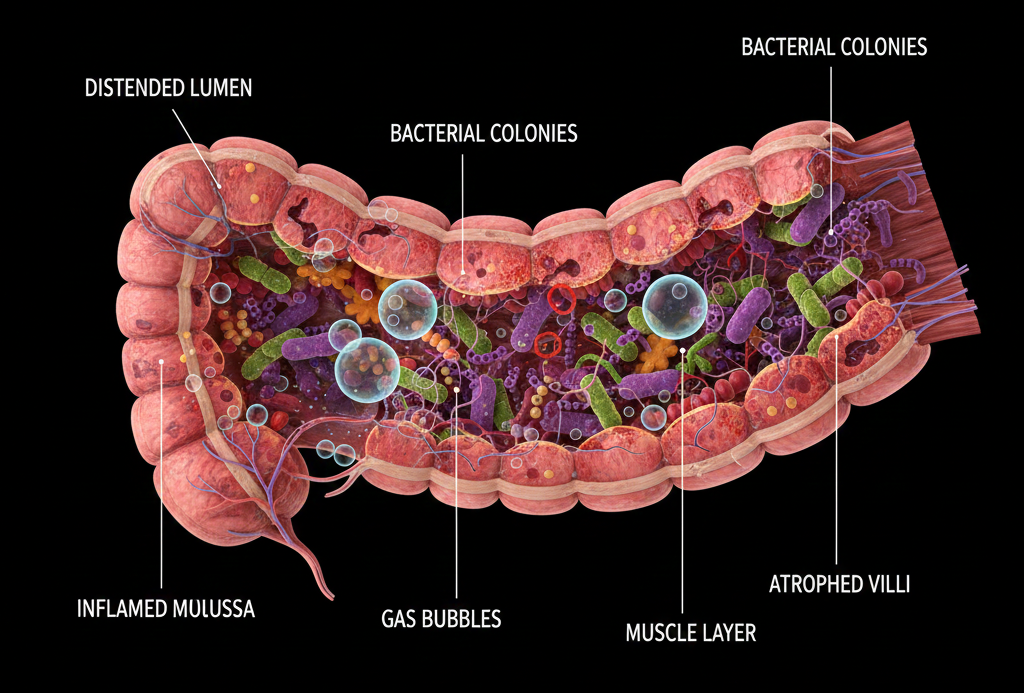
SIBO is a condition in which excessive bacteria grow in the small intestine, a part of the digestive tract that normally contains relatively few bacteria compared to the large intestine.
The small intestine is designed primarily for digestion and nutrient absorption, not bacterial fermentation. When bacteria multiply excessively in this region, they interfere with digestion by fermenting carbohydrates too early, producing gas and toxic byproducts that damage the intestinal lining and disrupt nutrient absorption.
Why Does Bacterial Overgrowth Occur?
SIBO is rarely a standalone disease. It usually develops as a secondary condition due to underlying problems that impair gut motility, anatomy, or defence mechanisms.
Key Causes of SIBO
- Impaired Gut Motility
The migrating motor complex (MMC) is a wave-like movement that sweeps bacteria out of the small intestine between meals. Conditions that slow motility—such as diabetes, hypothyroidism, or chronic stress—allow bacteria to accumulate. - Low Stomach Acid
Stomach acid acts as a natural disinfectant. Reduced acid production (due to aging or long-term acid-suppressing medications) allows bacteria to survive and migrate upward into the small intestine. - Structural Abnormalities
Surgical adhesions, diverticula, strictures, or blind loops can trap bacteria and promote overgrowth. - Damage to the Ileocecal Valve
This valve separates the small and large intestines. Dysfunction allows colonic bacteria to reflux into the small intestine. - Chronic Gastrointestinal Disorders
Conditions such as IBS, celiac disease, Crohn’s disease, and post-infectious gut syndromes are strongly associated with SIBO.
Types of SIBO
SIBO is now classified based on the dominant gas produced by bacteria, which influences symptoms and treatment response.
1. Hydrogen-Dominant SIBO
- Common symptoms: diarrhea, bloating, urgency
- Caused by carbohydrate-fermenting bacteria
2. Methane-Dominant Overgrowth (IMO)
- Common symptoms: constipation, slow transit, hard stools
- Caused by methane-producing archaea (not technically bacteria)
3. Hydrogen Sulfide SIBO
- Common symptoms: rotten-egg gas, diarrhea, nausea
- Less commonly tested but increasingly recognized
Common Symptoms of SIBO
SIBO symptoms vary widely in intensity and presentation, which is why it is often misdiagnosed.
Digestive Symptoms
- Persistent bloating (often worse after meals)
- Abdominal pain or discomfort
- Excessive gas or belching
- Diarrhea, constipation, or alternating bowel habits
- Acid reflux or nausea
Systemic Symptoms
- Chronic fatigue
- Brain fog
- Unintentional weight loss
- Nutrient deficiencies (iron, B12, fat-soluble vitamins)
- Skin issues and food sensitivities
Because bacteria consume nutrients before the body can absorb them, malnutrition and inflammation can develop even in individuals who eat well.
How Is SIBO Diagnosed?
Breath Testing (Gold Standard)
The most common diagnostic tool is a hydrogen–methane breath test. After ingesting a sugar solution (usually lactulose or glucose), breath samples are collected over several hours.
- Elevated hydrogen → hydrogen-dominant SIBO
- Elevated methane → methane-dominant overgrowth
While not perfect, breath testing is non-invasive and clinically useful when interpreted correctly.
Additional Diagnostic Clues
- Poor response to standard IBS treatments
- Temporary symptom relief with antibiotics
- Nutrient deficiencies without clear explanation
Treatment Options for SIBO
Effective SIBO treatment requires eliminating excess bacteria while correcting the underlying cause. Treating only symptoms often leads to relapse.
1. Antibiotic Therapy
Rifaximin
- Most commonly prescribed
- Poorly absorbed, acts locally in the gut
- Especially effective for hydrogen-dominant SIBO
Combination Therapy
- Rifaximin + other antibiotics may be used for methane-dominant cases
Antibiotics are typically given for 10–14 days, but recurrence is common without supportive strategies.
2. Herbal Antimicrobials
In some cases, botanical protocols using oregano oil, berberine, neem, or allicin are used as alternatives or adjuncts to antibiotics.
Studies suggest herbal regimens may be similarly effective when appropriately designed and monitored.
3. Dietary Management
Diet plays a critical role in symptom control and relapse prevention.
Low-FODMAP Diet
- Reduces fermentable carbohydrates
- Helps manage bloating and gas
- Not intended for long-term use
Elemental Diet
- Liquid, pre-digested nutrition
- Starves bacteria while nourishing the body
- Typically used for severe or refractory cases
4. Prokinetic Therapy
Prokinetics stimulate the migrating motor complex and are essential for preventing recurrence.
Examples include:
- Prescription motility agents
- Natural options such as ginger or specific serotonin modulators
Preventing SIBO Relapse
SIBO has a high recurrence rate, especially if root causes are not addressed.
Key Prevention Strategies
- Treat motility disorders
- Address thyroid or metabolic dysfunction
- Avoid unnecessary long-term acid suppression
- Space meals to allow MMC activity
- Support gut healing and nutrient repletion
SIBO and IBS: What’s the Connection?
Research increasingly suggests that a large proportion of IBS cases may be driven by SIBO, particularly post-infectious IBS. This explains why many IBS patients experience symptom relief after antimicrobial treatment.
However, SIBO is not the cause of all IBS, and careful diagnosis is essential.
Living With SIBO: A Long-Term Perspective
Managing SIBO requires patience, personalization, and professional guidance. There is no one-size-fits-all approach, and successful treatment often involves combining:
- Medical therapy
- Dietary adjustments
- Lifestyle changes
- Stress regulation
When treated comprehensively, many individuals experience significant improvement in quality of life, energy levels, and digestive comfort.
Final Thoughts
SIBO is a complex but highly treatable condition when properly understood. Awareness of its causes, accurate diagnosis, and a multi-layered treatment approach are key to lasting relief.
If you struggle with chronic bloating, unexplained digestive symptoms, or “IBS” that doesn’t respond to standard treatments, SIBO may be worth investigating with a qualified healthcare professional.